
Featured Resources
Fiscal Brief

August 2020
Federal Fix?
Aid From Washington May Keep Health + Hospitals Afloat,
For Now
PDF version available here.
Summary
After years on fiscal life-support, NYC Health + Hospitals was starting to see its budget stabilize. Then the Covid-19 pandemic arrived, straining the public hospital system’s ability to meet patient needs and cutting off revenue from elective surgery and other care. While NYC Health + Hospitals was able to close fiscal year 2020 with a cash balance of $688 million (enough for about a month of expenses), Health + Hospitals’ fiscal trajectory for 2021 and beyond is far less certain.
One key determinant of Health + Hospitals’ fiscal outlook is whether New York City suffers a resurgence of the virus. Another is whether the state continues to defer planned cuts to Medicaid, a primary revenue source for public hospitals that serve many uninsured and underinsured patients, as well as other potential cuts as Albany wrestles with its own budget shortfalls. A third determinant is the level of pandemic-related aid Health + Hospitals ultimately receives from Washington.
To date, there are four separate federal relief bills as well as other funding sources that can reimburse Health + Hospitals for pandemic-related costs and help address the revenue lost when the public hospitals were forced to turn away other patients to focus on the Covid-19 crisis. IBO has examined the federal legislation and has estimated how much funding assistance Health + Hospitals could receive. Among our key findings:
While this federal aid may be sufficient to help Health + Hospitals through the fiscal hurdles created by the pandemic in the near term, uncertainty remains longer term as the system is now losing about $25 million a week as admissions have declined and inpatient and outpatient services have not rebounded to pre-pandemic levels. A second surge of Covid-19 and/or a prolonged slowdown of New York’s economy could further deplete city and state tax collections, sparking cuts to major revenue sources for Health + Hospitals. Whether Washington would then provide additional relief remains highly speculative.
Covid-19’s Fiscal Impact on Health + Hospitals
In recent years, the fiscal condition of New York City Health + Hospitals (H+H) has been improving, allowing the system to build a modest cash balance. But the fiscal onslaught and uncertainty brought on by the Covid-19 pandemic and looming state Medicaid budget cuts threaten to undo that progress. Whether deterioration in H+H’s fiscal condition can be avoided will depend largely on how the pandemic plays out and H+H’s unique situation and strategy. It also will depend on how much emergency aid is made available by the federal government, the extent to which the pandemic eats into state and local revenues, and how the state addresses its own budget shortfalls.
This brief begins by reviewing the fiscal impact of the Covid-19 pandemic on the fragile fiscal condition of H+H. We then discuss what is known so far regarding the various forms of emergency financial assistance provided by the federal government that are expected to benefit H+H. While the promised federal assistance to H+H is likely to be substantial, the potential for major cuts to the state Medicaid program prompted by the state’s fiscal distress pose a significant threat to H+H’s finances.
Beginning in early March, as H+H began to plan and prepare for the anticipated Covid-19 surge that extended into mid-April, New York City hospitals were required to suspend elective surgery and nonessential care and expand bed capacity by at least 50 percent, leading to revenue losses, even as expenditures due to Covid-19 were increasing. These unprecedented changes have occurred in the context of an on-going shift in medical care delivery through hospital downsizing and the expansion of outpatient care, cuts to Medicaid and Medicare, with more anticipated, and growing state and city budget shortfalls.
To help hospitals weather this crisis emergency declarations by localities and states, and federal legislation, generated new government funding for many hospitals, including New York City Health + Hospitals. Most of the new revenue for hospitals comes from federal programs funded by the Coronavirus Aid Relief and Economic Security (CARES) Act and other federal legislation enacted since March, and from the Federal Emergency Management Agency (FEMA), which provides funding to address the immediate costs of treating and controlling Covid-19.1 The state also recently established a new fund to aid distressed hospitals and nursing homes and the New York State Department of Financial Services directed insurance plans to expedite hospital claim payments and help hospitals increase their liquidity.
As of July 30, 2020, Covid-19 has been responsible for over 56,132 hospitalizations and 23,525 confirmed and probable deaths in New York City. The disease disproportionately affected the city’s elderly; low-income; Black, Latino, and immigrant residents; members of large and multigenerational households; and individuals with one or more chronic health conditions. This epidemiology placed a heavy burden on H+H, which tends to serve a disproportionate number of nonwhite and immigrant individuals, many of whom lack health insurance. H+H also operates hospitals in some of the neighborhoods that were among the city’s worst Covid-19 hotspots.
Before the pandemic took hold in the city, H+H was expected to end city fiscal year 2020 with a closing cash balance of $790 million (unless otherwise noted, years refer to city fiscal years). These accumulated reserves put it in position to absorb some of the increase in expenses associated with Covid-19 and declines in reimbursement attributable to delayed/cancelled non-Covid-19 care. During the pre-Covid-19 preparation and surge period, H+H reported that its revenue losses due to Covid-19 were offset with increased admissions of Covid-19 patients. After the surge, however, H+H has been losing an estimated $25 million per week as the system continued to face higher expenses and fewer admissions.2 While both inpatient and outpatient utilization volume are starting to slowly rise, they have yet to rise to pre-Covid baseline levels.
Given the considerable uncertainty around the trajectory of the Covid-19 pandemic and availability of government funding, H+H has delayed issuing an updated financial plan. Thus, it will take time to fully understand the impact that Covid-19 will have on H+H’s health care delivery, utilization, and finances.
Increased Emergency Federal Funding Available For H+H, Although Amounts are Uncertain
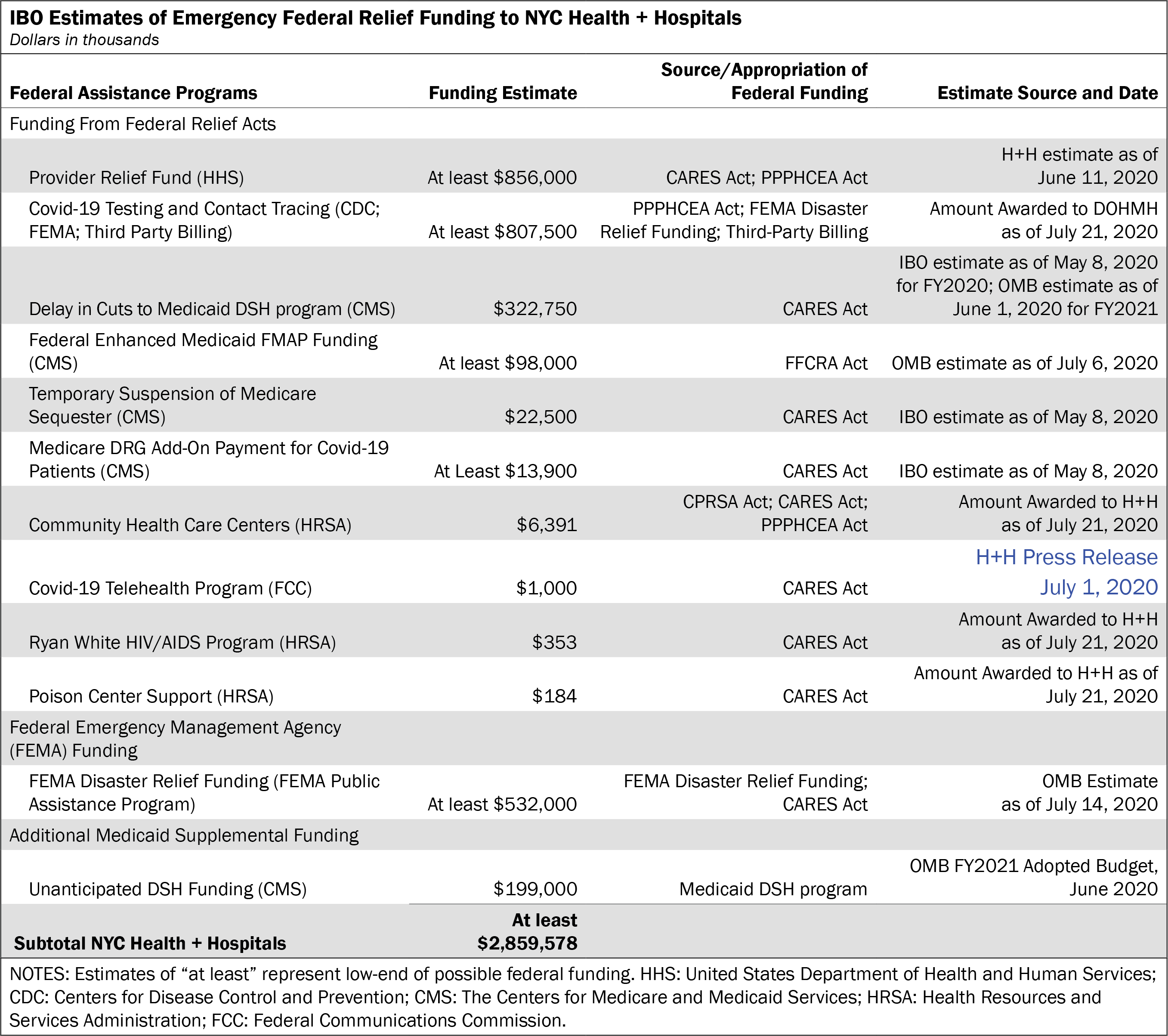
Federal emergency funding is providing significant financial assistance to hospitals in response to the Covid-19 pandemic. IBO estimates that federal Covid-19 emergency funding and relief packages enacted so far could provide a minimum of $2.8 billion to H+H.3 As discussed in an earlier IBO report, this is still a low-end estimate, with federal funding allocated to H+H expected to increase as further guidance and additional funding is released and/or new Covid-19 relief bills are enacted.
Federal Covid Relief Funding. Federal relief was authorized in four separate pieces of legislation. The first, the Coronavirus Preparedness and Response Supplemental Appropriations Act (CPRSA), 2020, was signed into law on March 6, 2020. The Families First Coronavirus Response Act (FFCR), was signed into law on March 18, 2020, and the Coronavirus Aid, Relief, and Economic Security Act (the CARES Act), was signed into law on March 27, 2020. It not only provides various health and economic assistance funding streams but also extends existing Federal Emergency Management Agency funding to be used to fight Covid-19. The most recently enacted legislation, the Paycheck Protection Program and Health Care Enhancement Act (PPPHCEA), was signed into law on April 24, 2020; the PPPHCEA Act supplements the CARES Act by providing additional funding for the program and greater flexibility for those tapping the assistance.4
Nationwide, the largest source of emergency assistance to hospitals is the Provider Relief Fund, which includes a total of $175 billion in funds for health care providers to cover the cost of Covid-19 related expenses and to replace revenue lost due to the pandemic; funding for the relief fund comes from the CARES Act ($100 billion) and the PPPHCEA ($75 billion). While IBO expects the Provider Relief Fund to be the largest source of assistance to H+H among the various components of the federal relief funding enacted so far, it is also still subject to some uncertainty as key allocation criteria and documentation requirements for distributing approximately $51.5 billion of funding still remain unclear. Congress delegated technical guidance and allocation decisions to the Department of Health and Human Services (HSS), which has been slowly releasing guidance and distributing funding. As of July 20, 2020, HSS has provided guidance for $123.5 billion of the $175 billion in funding. Allocations that H+H may be eligible for include a $50 billion “general allocation,” a $12 billion allocation for “Covid-19 high-impact areas,” which includes $2 billion for treatment of the uninsured, a $5 billion allocation for nursing homes, a $13 billion allocation to safety-net hospitals, and $10 billion for a second round of high impact area Covid-19 funding.
General allocation funding was first distributed back in April 2020 to Medicare fee-for-service providers across the country based on their 2018 share of net patient revenues.5 This distribution benefited providers that may have lost revenue as a result of the cancelation or delay of elective procedures and declines in outpatient care, but did not take into account the increased expenses incurred by providers who had to treat an overwhelming surge of Covid-19 patients. It also offered little assistance to safety-net hospitals, including H+H, whose patients are disproportionately uninsured or on Medicaid. To take account of these concerns, HSS began announcing a series of more targeted allocations that have been more favorable to H+H and New York City hospitals in general. In May, a total of $10 billion in funding for Covid-19 high-impact areas was allocated for hospitals that had provided inpatient care for 100 or more Covid-19 patients as of April 10, 2020. The $2 billion of high-impact area funding reserved for treatment of the uninsured was distributed to hospitals based on a fixed amount per Covid-19 inpatient admission with an additional amount taking into account hospitals’ Medicare and Medicaid disproportionate share and uninsured payments. On June 11, 2020, H+H reported receiving $824 million from the general allocation fund and the Covid-19 high-impact areas allocation, and is expecting up to $32 million for treatment of the uninsured.6 Given that there are other allocations from the provider fund that have not yet been costed by the system, IBO also expects H+H to receive additional funding from the Provider Relief Fund.
Another major source of federal funding is for Covid-19 testing and tracing. On May 8, 2020, Mayor de Blasio announced that H+H would be playing a lead role in administering the city’s Test and Trace Corps, a program that encompasses testing, contact tracing and providing care to individuals who need to be quarantined due to Covid-19, along with support from other city agencies. Most of the federal and other external funding for the program obtained by other city agencies or through grants or third-party billing will be funneled through H+H’s budget.7 This could include Centers for Disease Control and Prevention funding of approximately $807.5 million that has been allocated to the city health department from the PPPHCEA Act. FEMA funding can also be drawn down for testing. However, FEMA is a payer of last resort, so all other sources of funding need to be exhausted first.
The Families First Coronavirus Act included an enhanced Federal Medicaid Assistance Percentage (eFMAP) of 6.2 percent for Medicaid spending for the duration of the Covid-19 emergency declaration, which will get passed on to the city’s Medicaid budget. eFMAP savings include reductions to the weekly Medicaid payments the city makes to the state as part of its local contribution to the Medicaid program and savings for the city’s contribution to Medicaid supplemental payments. The city uses the latter mechanism to draw down additional federal matching Medicaid funds for H+H and effectively double the support given to the system. In the fiscal year 2021 Executive Budget, the de Blasio Administration estimated eFMAP savings would amount to approximately $489 million for the January to June 2020 period ($400 million in weekly payment reductions and $98 million in savings for supplemental Medicaid payments).8 However, on June 25th 2020, the state announced that eFMAP savings for weekly payments would only be $200 million.9 No federal guidance has been issued for eFMAP Medicaid supplemental savings, but the city is still expecting the $98 million to be paid. IBO’s $98 million estimate for eFMAP does not include any eFMAP savings H+H could receive from weekly Medicaid payment adjustments. The city can choose to apply these latter savings to its supplemental Medicaid share payments for H+H.
IBO estimates that H+H will receive a minimum of $345 million from two provisions in the federal relief acts that delay federal funding cuts to the Medicaid Disproportionate Share Hospital (DSH) program and a temporary suspension of a 2 percent cut to Medicare fee-for-service payments that was part of a 2013 Medicare savings initiative known as the Medicare Sequester. The DSH change will result in at least $323 million in savings to H+H and the suspension of the sequester cut will yield at least $22 million in savings.
The Medicaid DSH program provides additional Medicaid funds to providers who treat a disproportionate share of uninsured and Medicaid patients. Both cuts were previously set for May but have now been postponed until November 30, 2020.
Another potential revenue source for H+H is a 20 percent add-on to the Medicare fee-for-service diagnosis-related group (DRG) payment for Covid-19 discharges during the health emergency, which IBO estimates will increase H+H funding by nearly $14 million.10 Additional grants totaling roughly $7.9 million are expected from four smaller allocations.
Other provisions of aid bills are likely to provide additional funding for H+H, but are more difficult to estimate and are not included in the table on page 3, including free coronavirus testing for the uninsured through Medicaid and funding for community health centers that provide graduate medical education.
FEMA Funding. The March 13, 2020, national emergency declaration and March 20, 2020, disaster declaration for New York State has also enabled hospitals to receive Federal Emergency Management Agency funds for emergency protective measures related to Covid-19, such as emergency medical care and housing for those quarantined or isolated due to Covid-19 (medical sheltering). However, H+H cannot use FEMA funding to recover revenue lost due to the Covid-19 pandemic. FEMA funds for H+H flow through the city’s budget and the federal government typically reimburses 75 percent of costs, although Governor Cuomo has told the press that he received verbal assurance from the President that the state will receive 100 percent federal reimbursement. H+H is eligible to apply for FEMA reimbursement and submitted an initial claim for $650 million on March 27, 2020. As of July 14, 2020, H+H has been approved for $532 million, but has not yet received any disbursements. H+H has subsequently revised their estimate of reimbursable expenses upwards to $1.1 billion. If the state does not receive 100 percent of federal funding, H+H will be required to pay 25 percent of FEMA approved costs.
Unanticipated Medicaid Supplemental Funding. The city’s 2021 Adopted Budget included an additional $199 million in unanticipated DSH payments to H+H for 2020. The money was transferred from H+H’s subsidy budget to the city’s supplemental Medicaid budget allowing the funds to be used to draw down the same amount of federal Medicaid payments going to H+H, doubling the city’s contribution.
A State of Funding Uncertainty
While considerable funding is available for hospitals at the federal level, potential cost-cutting measures for hospitals are on the horizon at the state level. New York State was already facing budget shortfalls before the Covid-19 pandemic hit. The state fiscal year 2021 Executive Budget identified a $6 billion budget gap, and a panel of industry stakeholders known as the Medicaid Redesign Team II (MRT II) were tasked with finding $2.5 billion in Medicaid savings for 2021. MRT II recommended a total of $1.6 billion in savings, of which nearly $1.5 billion was included in the enacted budget, relegating further cost cutting measures to the future.11
Some of the cost cutting measures will affect H+H, such as a 1.5 percent across-the-board cut in Medicaid payments, which began in January, as well as cuts to quality pools for managed care and hospitals and capital reimbursement to hospitals and nursing homes. As part of the MRT II recommendations, H+H is currently working with the state to improve the equity of Medicaid supplemental funding through indigent care pool redistributions and the sustainability of such funding by converting Medicaid supplemental payments into Medicaid rate increases. The hope is that any incremental revenue for H+H can exceed state Medicaid reimbursement cuts. However, any approved MRT II initiative that affects Medicaid eligibility standards, methodology, or procedures, such as the initiatives aimed at containing costs in long-term care, are unlikely to have a near-term impact on H+H’s finances. This is because under the legislation, a state cannot receive a temporary increase in its federal share of Medicaid costs (eFMAP) unless it refrains from making such changes while eFMAP is in effect.12
The adopted state budget adds to the uncertainty regarding Medicaid funding by granting the Governor authority to institute further mid-year cuts in at three points in the fiscal year (May, June, and January) if gaps emerge in the state budget. The state currently has a budget deficit of $14.5 billion, according to the latest estimate from the Governor’s office. The Governor has said that unless the state receives additional federal aid, the state will have to cut public programs and services, if necessary by using the Governor’s newly granted cutting authority (the State Legislature has 10 days to propose and enact alternative cuts). Medicaid and education are the biggest components of the state budget, so if cuts happen, Medicaid reductions would be virtually unavoidable. H+H has estimated that if the state’s $13.3 billion deficit is applied across all state programs, it will amount to a 20 percent cut to the Medicaid.
In addition to the uncertainty resulting from this year’s state budget process, because Medicaid caseloads and spending increase during periods of high unemployment when state revenues are typically shrinking, there will likely be additional pressure on the state to find even more savings in the Medicaid program if the current recession persists. This will be particularly true if Medicaid enrollment increases are not matched by extra federal Medicaid funding to make up for Covid-19 expenses.
In the past, H+H has been able to leverage additional external funding using Medicaid waiver funding programs. However, these revenue sources are set to decline as two of the programs, the Delivery System Reform Incentive Payment program (DSRIP) and the Care Restructuring Enhancement Pilots, are scheduled to end. Extension of these programs would improve H+H’s financial outlook, but require state and federal approval. The federal Centers for Medicare & Medicaid Services (CMS) has denied the state’s request for an extension of DSRIP, and the program ended on March 21, 2020.
Due to the Covid-19 pandemic, however, CMS has introduced a number of new waiver authorities, including developing a section 1115 demonstration to provide opportunities for states to have more flexibility to modify their Medicaid programs to improve enrollment and deliver care during the Covid-19 emergency. The state Department of Health submitted a section 1135 waiver and other requests to amend its Medicaid eligibility and enrollment policies to make it easier for recipients to qualify and stay on Medicaid. The state has also submitted a 1115 waiver requesting more than $2.7 billion in new federal funding for the period March 1, 2020-March 31, 2021 to respond to the Covid-19 pandemic. The waiver aims to repurpose infrastructure established under DSRIP to promote regional coordination and investments in telehealth infrastructure, and support health care system transformation activities, including the rapid repurposing of facilities to meet surge capacity demands.13 This waiver still needs federal approval. It is currently unclear whether any of its components will be approved as the proposal is costly and more expansive than the model programs described by CMS in its template application.
In anticipation of the effects that Covid-19 will have on health providers, the state fiscal year 2021 enacted budget established a fund for distressed hospitals and nursing homes. However, it is still unclear which institutions will receive these funds or how the funds will be distributed. H+H is likely to receive some of this funding. The initiative is funded in part by a state intercept of the city’s sales tax revenue, which will cost the city approximately $400 million over a two-year period ($250 million in city fiscal year 2021 and $150 million in 2022).
A Difficult Prognosis
It will take time to understand the impact that Covid-19 has had on the public hospital system. That assessment will depend not only on H+H’s unique factors (its patient and case mix, hospital capacity and recovery strategies) but also on external factors such as Covid-19 pandemic case rates, state and city approaches to reopening the economy, regulations around resumption of elective surgeries and social distancing, and progress in finding an effective treatment or vaccine for the virus. For H+H in particular, its outlook is dependent on continued city and state support, which in turn is dependent on additional federal aid.
Currently, Covid-19 cases have been rapidly increasing around the country, increasing the risk of another surge of cases in New York. If such a scenario materializes, even if it is not as grave as what happened in March and April of this year, it will have consequences for H+H due to the reduced inpatient and outpatient utilization the system is currently experiencing compared with its baseline. In addition, the public hospital system would need to absorb Covid-19 related costs while facing potential state Medicaid and city budget cuts. A second surge or shutdown could also further deplete city and state’s resources, further hindering support to the Medicaid program and H+H.
Report prepared by Melinda Elias
PDF version available here.
Endnotes
1The federal government also extended the Medicare accelerated payment program, which provides qualified hospitals up to a six month advances on lump-sum and periodic payments. This is a loan, not a grant. However, a hospital is not required to start paying down the loan for 120 days (four months) and also has at least 12 months to complete repayment.
2H+H’s president discussed the weekly losses during a town hall meeting with Assemblyman Richard Gottfried on June 27th. https://subscriber.politicopro.com/states/new-york/whiteboard/2020/07/27/nyc-health-hospitals-ceo-system-losing-25m-a-week-due-to-pandemic-9423739. Previously, H+H at its most recent Finance Committee meeting on June 11 reported that losses had averaged $23 million per week between April 19 and May 23.
3This amount does not include the funds allocated in addition to existing FEMA Disaster Relief funding that was appropriated as part of the CARES Act.
4Negotiations are currently underway on an additional stimulus/relief bill.
5Initially $20 billion was disbursed based on Medicaid fee-for-service payments in 2019. However the $30 billion made allocations to even out payments to make reimbursement based on share of net patient revenue.
6For Provider Relief Fund COVID-19 High Impact Payments see: https://data.cdc.gov/Administrative/Provider-Relief-Fund-COVID-19-High-Impact-Payments/b58h-s9zx For payments provided to hospitals from the $50 billion general distribution allocation see https://data.cdc.gov/Administrative/HHS-Provider-Relief-Fund/kh8y-3es6 Accessed July 27, 2020 with content last reviewed on July 20 and July 24, 2020, respectively.
7A new budget code (CV01) has been established in H+H’s budget for Covid-19 testing and tracing. It is envisioned that this code will be used to identify most of the funding for testing and tracing. Initially, not all funding will be added to this code, but H+H will be able to draw down funding as needed.
8The total amount of eFMAP savings the city estimates receiving is $942 million for the period January to December 2020.
9In the 2021 Executive Budget, $498 million was added in miscellaneous revenue for 2020 ($400 million as weekly payment reduction and $98 million for supplemental Medicaid payments) and the Medicaid budget was also reduced by $444 million in 2021 to account for all 12 months of calendar year 2020. However, the state recently announced that there would only be $201 million of eFMAP savings to weekly payments as opposed to $400 million of eFMAP savings for the first six months of calendar year 2020,of which 80 percent ($161 million) will be passed as adjustments to the city’s weekly Medicaid payments starting in July 2020. As of July 6, 2020, the city is still expecting to receive the $200 million shortfall from weekly payments from the state for 2020 and $98 million for supplemental Medicaid payments to be paid retroactively in 2020. The 2021 Adopted Budget takes down $361 million of miscellaneous revenue in 2020 from the revenue budget (keeping just 20 percent of the $201 million and $98 million for supplemental Medicaid payments in 2020). The city’s Medicaid budget was also further reduced for 2021 by $161 million (total reduction for 2021 now being $604 million in eFMAP savings), to reflect deferred eFMAP savings from 2020, which can now be used for other city spending in 2021. However, the city did not take downthe $200 million of savings it expects to receive from the 2020 shortfall to 2021 yet.
10See IBO report “How Much “CARE” for NYC? An Estimate of Federal Coronavirus Emergency Relief Act Funding to the City Budget” for more information on how that estimate was derived. https://ibo.nyc.ny.us/iboreports/how-much-CARE-for-nyc-an-estimate-of-federal-coronavirus-emergency-relief-act-funding-to-the-city-budget-may-2020.pdf
11Note: this does not include an additional $739 million in Medicaid administrative cost savings that were enacted as part of the Medicaid savings plan.
12The state budget includes language that allows the MRT II actions to be delayed up to 90 days after the State’s COVID-19 emergency is over.
13Funding requested would expire either on the state’s proposed end date of March 31, 2021, or 60 days after the currently declared public health emergency ends. The waiver also requests to extend the current MRT demonstration waiver up to 12 months.